Design and development of a novel infrastructure to securely share radiation therapy data through direct patient data sharing
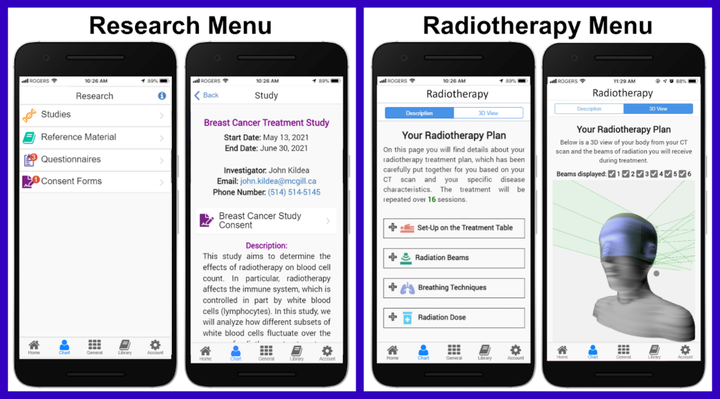 Image credit: Kayla O’Sullivan-Steben
Image credit: Kayla O’Sullivan-StebenAbstract
Introduction: With the rise of precision medicine and use of artificial intelligence in radiation oncology, researchers increasingly need access to large amounts of real-world data from a variety of patients. While these data exist, they are typically legally protected and spread across multiple databases and institutions. Patients, like researchers, need access to their data, as knowledge about one’s disease and treatment leads to reduced anxiety and potentially better treatment outcomes. This project addresses both needs by giving patients access to their radiotherapy data and control over who they can share them with for research. The goal was to create the patient-facing component of a patient-centric data-sharing platform based on the Opal patient portal (opalmedapps.com) that will engage and empower radiotherapy patients to contribute data to research. Methods: Following a participatory stakeholder co-design approach, data sharing was facilitated by the addition of two new JavaScript user interfaces to the Opal app: a Radiotherapy menu and a Research menu. To display patient data in the Radiotherapy menu, treatment plan data were first extracted from DICOM-RT Plan and Structure Set files. Treatment parameters were contextualized with explanatory text, and an algorithm was created to render the patient’s body contour data and beam configurations in 3D. Next, to allow patients to participate in research within the app, the Research menu was built to receive and display study invitations, surveys, and related information from researchers. An electronic consent form feature requiring password input was also implemented to obtain patient consent securely. Finally, a patient focus group was conducted to gather initial patient feedback on the new menus. Results: The Radiotherapy menu presents a customized explanation of a patient’s treatment plan based on their treatment parameters. The text is organized into four main categories: patient positioning, radiation beams, breathing techniques and radiation dose. The menu also displays an interactive 3D rendering of the patient’s body and planned treatment beams for visualization, which can be interacted with using smartphone touch gestures. Next, the Research menu lists ongoing studies, relevant reference materials, research questionnaires and electronic consent forms. Patients who consent to a given study will be able to answer questionnaires from researchers and receive updates and results about the studies they join through the app. Finally, the focus group feedback was overwhelmingly positive. By presenting complex radiotherapy data in an intuitive manner, patients will likely be better prepared for their radiation treatments and will be more willing to share their data with researchers. Conclusion: By prioritizing patient education and access to data, the data-sharing platform created in this project uniquely fosters an important sense of trust between the patient and researcher that will empower patients to confidently and enthusiastically contribute their data to research. This platform has the potential to help further Big Data efforts in medical research.