Retrospective evaluation of the effects of interobserver contouring practices in clinical practice
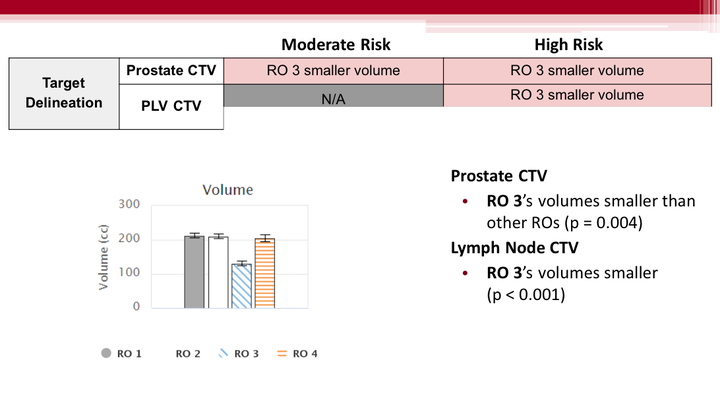 Image credit: Haley Patrick
Image credit: Haley PatrickAbstract
Purpose: To assess the contouring practices of radiation oncologists during everyday clinical practice and their impact on patient DVHs at a population level.
Materials and Methods: The DVHs of 560 prostate cancer patients who had undergone hypofractionated treatment (60Gy in 20 fractions) were exported from the Eclipse treatment planning system (Varian Medical Systems, Palo Alto, CA) into a custom DVH registry at our institution along with structure volumes and lengths. Patients were separated into intermediate (prostate only) or high-risk (additional 44Gy boost to pelvic lymph nodes) cohorts and further categorized based on primary radiation oncologist (RO). Structure volumes, lengths, and DVHs were compared between oncologists using 2-tailed Student’s t-tests.
Results: PTV coverage was consistent across ROs and risk levels. In intermediate risk patients, no differences in contouring habits or DVH distributions were observed. However, in high-risk patients, one radiation oncologist achieved significantly more sparing of the rectum and bladder than their peers. The root cause was determined to be an inconsistent pelvic lymph node contour definition between ROs. The RO achieving better sparing contoured significantly smaller lymph node CTVs than their peers, and two other ROs adhered to different cranial-caudal limits than others. In light of these findings, we presented our results to the oncologists at our institution, prompting the selection of a universal pelvic lymph node contour definition.
Conclusions: Systematic interobserver contouring practices in regular clinical practice are detectable through statistical analysis of past treatment plans. Retrospective revision of these practices is recommended as a quality assurance measure to ensure consistent quality of care across an institution.