A Scalable Radiomics- and Natural Language Processing–Based Machine Learning Pipeline to Distinguish Between Painful and Painless Thoracic Spinal Bone Metastases: Retrospective Algorithm Development and Validation Study
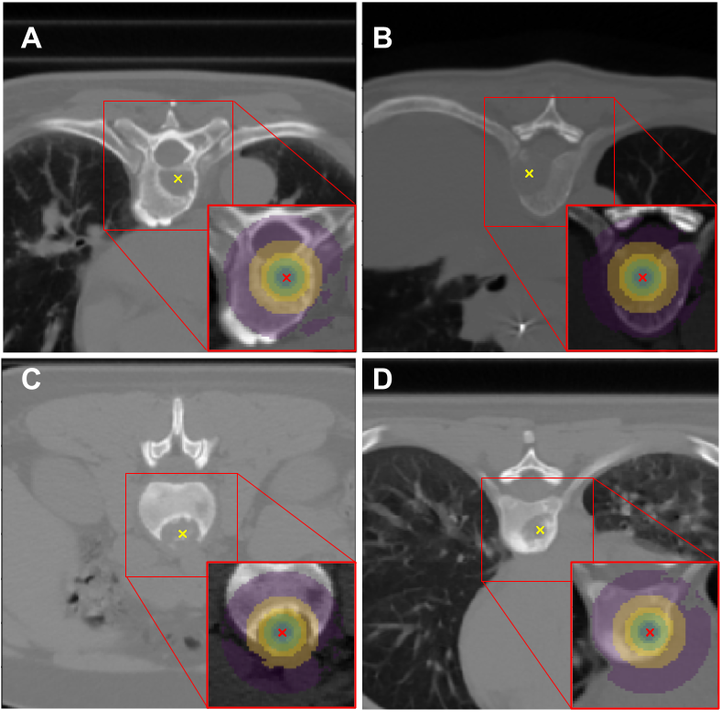 Image credit: Hossein Naseri
Image credit: Hossein NaseriAbstract
Background: The identification of objective pain biomarkers can contribute to an improved understanding of pain, as well as its prognosis and better management. Hence, it has the potential to improve the quality of life of patients with cancer. Artificial intelligence can aid in the extraction of objective pain biomarkers for patients with cancer with bone metastases (BMs). Objective: This study aimed to develop and evaluate a scalable natural language processing (NLP)– and radiomics-based machine learning pipeline to differentiate between painless and painful BM lesions in simulation computed tomography (CT) images using imaging features (biomarkers) extracted from lesion center point–based regions of interest (ROIs). Methods: Patients treated at our comprehensive cancer center who received palliative radiotherapy for thoracic spine BM between January 2016 and September 2019 were included in this retrospective study. Physician-reported pain scores were extracted automatically from radiation oncology consultation notes using an NLP pipeline. BM center points were manually pinpointed on CT images by radiation oncologists. Nested ROIs with various diameters were automatically delineated around these expert-identified BM center points, and radiomics features were extracted from each ROI. Synthetic Minority Oversampling Technique resampling, the Least Absolute Shrinkage And Selection Operator feature selection method, and various machine learning classifiers were evaluated using precision, recall, F1-score, and area under the receiver operating characteristic curve. Results: Radiation therapy consultation notes and simulation CT images of 176 patients (mean age 66, SD 14 years; 95 males) with thoracic spine BM were included in this study. After BM center point identification, 107 radiomics features were extracted from each spherical ROI using pyradiomics. Data were divided into 70% and 30% training and hold-out test sets, respectively. In the test set, the accuracy, sensitivity, specificity, and area under the receiver operating characteristic curve of our best performing model (neural network classifier on an ensemble ROI) were 0.82 (132/163), 0.59 (16/27), 0.85 (116/136), and 0.83, respectively. Conclusions: Our NLP- and radiomics-based machine learning pipeline was successful in differentiating between painful and painless BM lesions. It is intrinsically scalable by using NLP to extract pain scores from clinical notes and by requiring only center points to identify BM lesions in CT images.