Predicting radiotherapy replanning for head and neck cancer
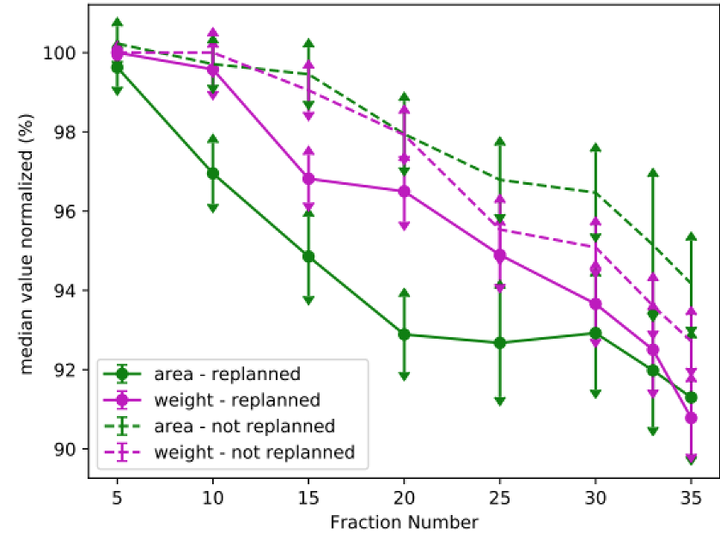 Image credit: Kayla O’Sullivan-Steben
Image credit: Kayla O’Sullivan-StebenAbstract
Introduction: Head and neck cancer patients undergoing radiotherapy often experience weight loss over the course of treatment due to the effects of radiation. This weight loss can result in anatomical changes within the head and neck region (Figure 1) such that the dose distribution planned using the simulation CT no longer respects the dose constraints of the organs at risk (OARs). When this is the case, the patient must have their treatment replanned to account for the anatomical changes and to ensure acceptable dose is delivered to the tumour and the OARs. At the McGill University Health Centre, decisions surrounding patient replanning are made based on visual inspection of CBCT scans taken for the purposes of Image-Guided Radiotherapy (IGRT), as well as on quantitative analysis of the dose distribution changes. Currently, this monitoring process is carried out ad hoc, which often leads to replanning decisions being made with short notice to the planning team. Because head and neck cancer treatment plans tend to be complex and require fast turnaround, this last-minute decision-making process can significantly disrupt the workflow of the planning team, which may in turn affect the timeline of other patient treatments. It would therefore be beneficial to pre-emptively determine if and when a patient will need replanning.
Objectives: Our research team’s overarching goal is to develop a predictive model that will facilitate head and neck replanning decisions. The objective of our work to date is to predict whether or not patients will need replanning based on clinical data from the start of treatment and weight-loss and IGRT imaging data taken over the course of treatment. As we move this project forward, our objective will be to predict the anatomical changes themselves that a patient will experience over the course of their treatment using a digital twin framework that will dynamically update as new data are collected for the patient. This talk will provide an overview of our research group’s past and future directions towards pre-emptive head and neck radiotherapy replanning.
Previous Work: Previous work conducted by our research group began by examining the correlation between body mass loss related metrics and replanning decisions. The result of this initial research was the identification of a temporal imaging-derived metric that is (imperfectly) predictive of patient replanning. This metric relates to the rate of change of the minimum distance xmin between the planning target volume (PTV) and the patient’s skin (Figure 1). Recently, our group has begun implementing machine learning classification models that incorporate this metric along with demographic and tumour characteristics data to predict head and neck cancer radiotherapy replanning.
Future Directions: To date, aside from the xmin parameter extracted from patients’ CBCT scans, the information in the images themselves has not been directly incorporated into our predictive models, partially due to its high-dimensionality. To overcome this issue, our next step will be to employ deep learning-based dimensionality reduction that will allow us to more easily work with these imaging data while still preserving their most important features. Specifically, we will train an autoencoder – a neural network composed of an encoder and decoder – to learn to condense CBCT imaging data into vector representations in a lower-dimensional latent space. For each patient, their data will be encoded in latent space and the trajectory describing the change in their CBCT scans over the course of radiotherapy will be mapped in this space (Figure 2a). We hypothesize that we will then be able to accurately predict the trajectory of anatomical changes for new patients within the latent space. To do this, we will encode a patient’s data into latent space at the start of treatment and subsequently extrapolate their most probable trajectory based on past patients that neighbour them in latent space (Figure 2b). Points along the trajectory will then be decoded to reconstruct the predicted CBCT scans. Finally, we aim to incorporate a digital twin framework whereby patient trajectories will be dynamically updated based on new data collected over the course of treatment. This will improve our ability to predict if and when a head and neck cancer patient will need replanning.